Patient Derived Cell Assays – The Case
The annual number of new drug approvals is trending upwards, the number of 'first-in-class' therapies has remained relatively constant — often fewer than 10 per year. For such new medicines for 'pioneer targets', attrition in Phase II proof-of-concept clinical studies remains the biggest hurdle1, in large part because the target–disease associations derived from the currently dominant cell-line or animal preclinical models of disease often do not translate into clinical efficacy.
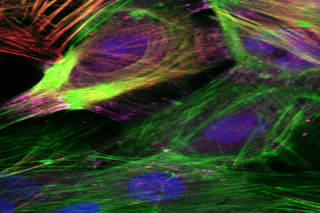
It is increasingly appreciated that the use of disease models based on human samples is critical both to increase our understanding of pathophysiology and to reduce clinical attrition. However, securing regular access to well-annotated samples from patients is challenging to organize and raises ethical issues.
The ULTRA-DD project has been funded to directly address these issues.
- Disease models - cell lines and animal - often poorly predict disease
- The ultimate model should be tissue/cells from the human disease
- Access to patient cells and tissue has been the key in inflammation; to define and validate new drug targets in relevant cells and context, e.g. for:
- Anti-TNF and
- Anti-IL17 therapies
- We are now building a scalable new organisation to recapitulate such successes
- This partnership, starting formally March 1st 2015, comprises Universitites, Hospitals, Pharmaceutical Companies, Biotechs and Disease Foundations
More information:



